Endometriosis and women’s quality of life: A comprehensive approach to disease management.
Introduction
Endometriosis is not just a physical condition; it has a wide-ranging impact on women’s mental health, quality of life, and social relationships. Chronic pain, infertility, and emotional problems reduce life satisfaction and daily productivity. Management of this condition must go beyond treating physical symptoms and address psychological and social aspects as well.
Physical effects
1. Chronic pain
-
Severe pelvic pain and dysmenorrhea.
-
Pain during sexual intercourse (dyspareunia).
-
Chronic menstrual pain that disrupts daily life.
2. Infertility
-
About 30 to 50 percent of women with endometriosis experience fertility problems.
-
Increased anxiety and stress caused by unsuccessful attempts to conceive.
Psychological effects
1. Anxiety and depression
-
Constant worry about the severity of the pain and the progression of the disease.
-
Feeling helpless and unmotivated.
2. Decreased self-confidence
-
Body changes, sexual limitations, and fertility all contribute to a diminished self-image.
3. Sleep problems
-
Chronic pain causes sleep disturbance and chronic fatigue.
Social impacts
-
Limitation of social and work activities.
-
Pressure on marital and family relationships.
-
Feelings of isolation and reduced participation in society.
Comprehensive disease management
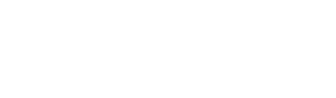
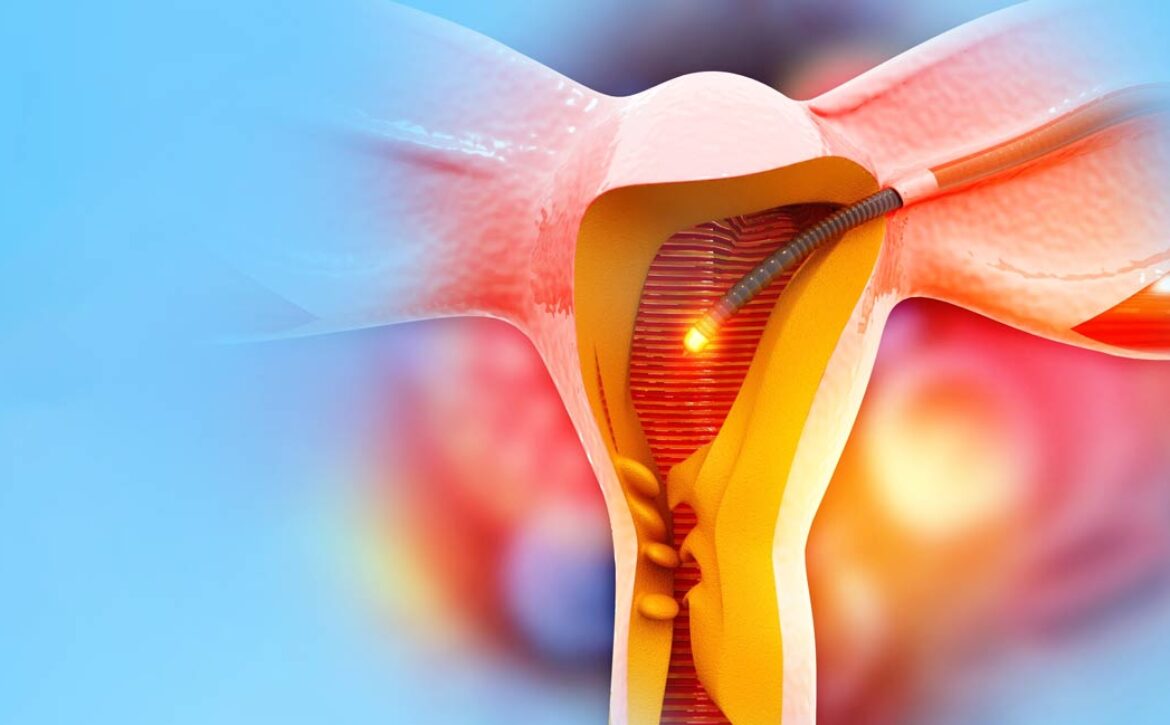
1. Medical treatment
-
Medication, surgery, and combination therapies to control physical symptoms.
2. Psychological support
-
Individual and group counseling for managing anxiety and depression.
-
Cognitive-behavioral psychotherapy (CBT) techniques.
3. Lifestyle and physical activity
-
Regular exercise and physical activity to reduce pain and improve mood.
-
Healthy eating and anti-inflammatory diet.
4. Support groups
-
Connecting with other women with endometriosis.
-
Exchange of experience and psychological support.
5. Pain management and complementary methods
-
Yoga, meditation, and acupuncture to reduce pain and stress.
Conclusion
A multidimensional approach is essential to improve the quality of life of women with endometriosis. This approach must consider both the physical health, mental health, and social relationships of women. Successful treatment is not limited to pain relief; it also includes psychological support, lifestyle modifications, and the creation of a social support network.
Suggested References
-
Human Reproduction Update (2024): Impact of endometriosis on quality of life
-
Fertility and Sterility Journal: Psychological and social aspects of endometriosis